Leishmaniasis is a chronic inflammatory parasitic disease transmitted through the bite of infected sandflies. Visceral (VL), Cutaneous (CL) and Mucocutaneous (ML) are the 3 major forms of the disease which affects around 1 million annual new cases globally. The disease is most prevalent among the poor and shows association with malnutrition, population displacement, poor housing and weak immunity. Prevalence of Leishmaniasis has seen a gradual increase in Sri lanka with over 200,000 annually recorded patients at different disease stages. Therefore, early diagnosis and effective case management will help significantly reduce the disease prevalence and associated disabilities including death. Clinical features of skin lesions, microscopic examination of skin lesion, splenic /bone marrow/lymph node aspirates, and molecular diagnostics based on PCR are used for differential diagnosis of the disease.
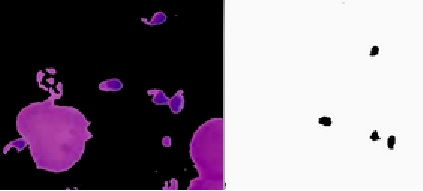
Advancements in diagnostics, chemotherapeutics and vector control are critical for effective management and control of this infection.The disease progression of VL is considered serious and if untreated leads to systemic and progressive infection of macrophages in the reticulo-endothelial systems or lymphoid organs (spleen, liver and bone marrow). Clinical manifestations of VL include hepatosplenomegaly, fever, anemia, leucopenia, hypergammaglobulinemia and cachexia. Parasitologic diagnosis is still considered the gold standard in Leishmaniasis diagnosis because of its high specificity. Identification of amastigotes in stained lesion smears is used for differential diagnosis of CL and ML. For example in CL, amastigotes appear as round or oval bodies, about 2–4 µm in diameter, with characteristic nuclei and kinetoplasts. Histopathological investigation of splenic or bone marrow aspirates are used for diagnosis of VL.